Coronavirus
- Thread starter C.B. Brown
- Start date
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Found two interesting articles about the border being closed due to COVID-19 and it’s eventual opening. First one is saying how if NHL players can cross the border to play hockey why not travelers. And the second article is about Maine opening it’s border with New Brunswick.
News about the second shot in Quebec
This one could also go in the NHL thread but I thought it was more fitting here because it has to do more about COVID than it does about hockey IMHO. If the 2 countries have figured out how to have hockey teams cross the borders many are going to be pissed off that it doesn't apply to regular people. Because of their relation to the NHL people on these teams can cross borders but for regular folks we must still wait and see. Don't get me wrong, I'm happy about this, but it's also bullshit that we can make this happen for sports but not for regular citizens that have suffered because of the border closure. Obviously not me, I just want the border opened for my own personal horny gains.

 www.espn.com
www.espn.com

NHL, Canadian government reach agreement for cross-border travel ahead of Stanley Cup semifinals
The NHL has reached an agreement with the Canadian government to allow for cross-border travel beginning with the Stanley Cup semifinals, the league announced on Sunday.
NY Governor Cuomo announced that when 70% of NY'ers have received at least one shot of the COVID vaccine he will lift "virtually all" COVID related restrictions. Currently NY is at 68.6 percent:

 nypost.com
nypost.com

Gov. Cuomo: COVID restrictions will be lifted when 70 percent of New Yorkers are vaxed
Gov. Andrew Cuomo promised that he will lift “virtually all” COVID-19-related restrictions once 70 percent of New York State residents have received a jab.
NY Governor Cuomo announced that when 70% of NY'ers have received at least one shot of the COVID vaccine he will lift "virtually all" COVID related restrictions. Currently NY is at 68.6 percent:

Gov. Cuomo: COVID restrictions will be lifted when 70 percent of New Yorkers are vaxed
Gov. Andrew Cuomo promised that he will lift “virtually all” COVID-19-related restrictions once 70 percent of New York State residents have received a jab.nypost.com
Hard to believe but Quebec is at 72.8 according to this

As Quebec vaccinations rise, health authorities open small clinics to improve access to Montreal communities
Over 75 percent of adult Quebecers have received one dose of a COVID-19 vaccine. But in some areas of Montreal and Laval, that number isn't quite as high.
Possibly NY is opening up because of the one shot percentage combined with the fully vaccinated numbers as well. Which may not really matter because the CDC recently posted that with at least one shot of the Pfizer or Moderna vaccine the effective rate was 81%. All good news across the board:Hard to believe but Quebec is at 72.8 according to this

As Quebec vaccinations rise, health authorities open small clinics to improve access to Montreal communities
Over 75 percent of adult Quebecers have received one dose of a COVID-19 vaccine. But in some areas of Montreal and Laval, that number isn't quite as high.montreal.ctvnews.ca
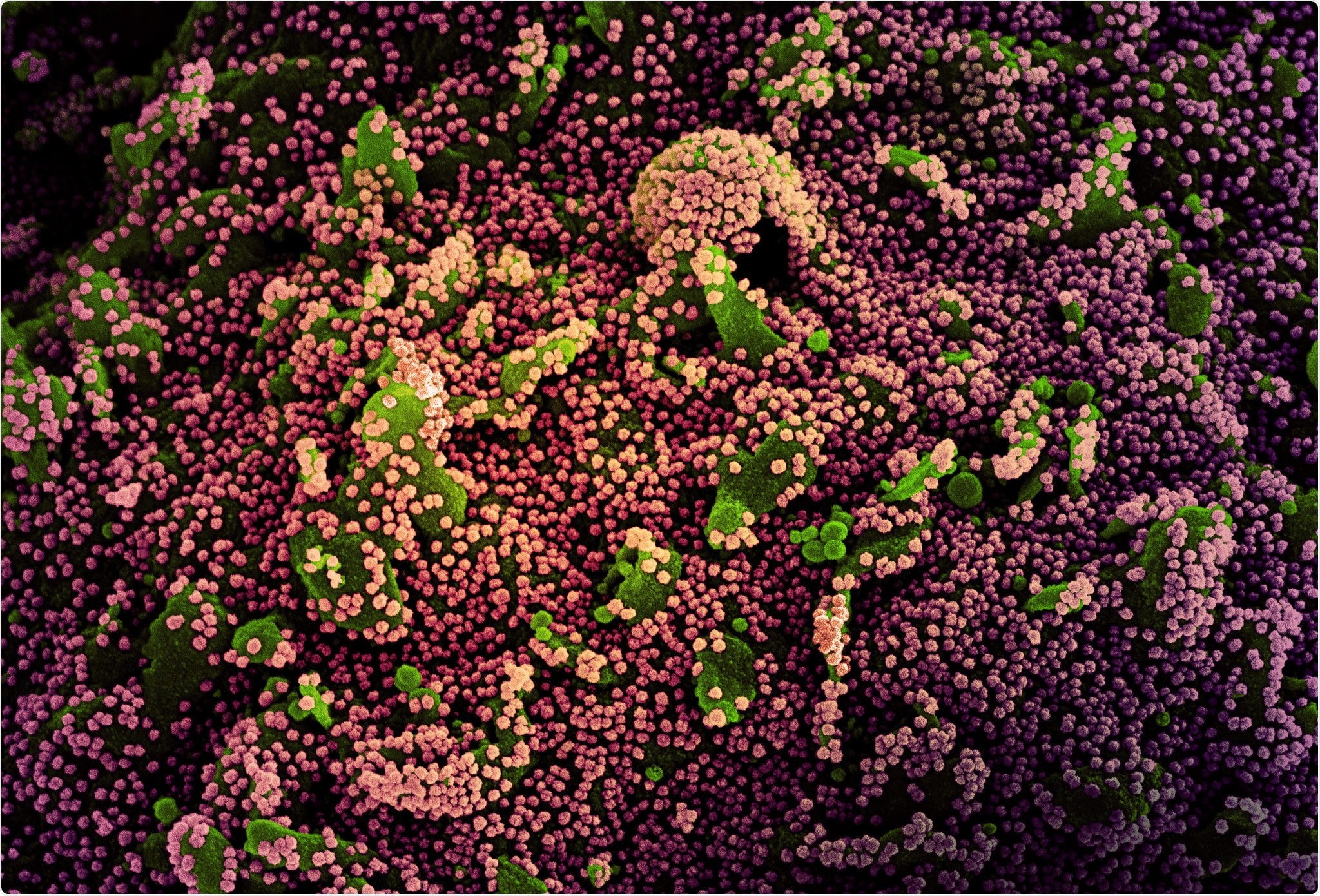
New data from CDC on effectiveness of Pfizer and Moderna COVID-19 vaccines
Researchers in the United States have conducted a study demonstrating the real-world effectiveness of the Pfizer-BioNTech and Moderna coronavirus disease 2019 (COVID-19) vaccines at preventing infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Possibly NY is opening up because of the one shot percentage combined with the fully vaccinated numbers as well. Which may not really matter because the CDC recently posted that with at least one shot of the Pfizer or Moderna vaccine the effective rate was 81%. All good news across the board:
New data from CDC on effectiveness of Pfizer and Moderna COVID-19 vaccines
Researchers in the United States have conducted a study demonstrating the real-world effectiveness of the Pfizer-BioNTech and Moderna coronavirus disease 2019 (COVID-19) vaccines at preventing infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).www.news-medical.net
yes. Agreed
But this is what we have to watch out for : Delta
The variants were given new "code names" Alpha is the first "British Variant, the one for the South African, another for the Brazilian and now "Delta" is the Indian version
A single dose of Pfizer was 80% effective on the original but only 32% on Delta.
Many places are still mostly dealing with the original strain so that 80% holds. But if Delta breaks out, all bets are off. This is why the government is pushing so hard to get the second dose injected.
This is why the UK, who was ahed of everyone (including the US) is now reconsidering their opening up.
The game is changing fast and the rules 2 months ago, no longer apply.
This is why I cringe when I see celebrations like last night. If the Indian variant is here, we're f'd. The government is doing a great job trying to re-energize a very tired population, but this war isn't over.
If we open up smart, we can guarantee to stay open. Too fast and we'll be back in confinement.
We will now have to deal with the '' variant plus '' more contagieux.......so une autre raison pour être doublement vacciné asap. 

As Delta Variant Surges, Outbreaks Return in Many Parts of the World (Published 2021)
The highly contagious Delta variant is on the rise, and countries that hoped they had seen the worst of Covid-19 are being battered again.
As Delta variant surges, outbreaks return in many parts of the world.
The highly contagious Delta variant is on the rise, and countries that hoped they had seen the worst of Covid-19 are being battered again.
The nightmare is returning.
In Indonesia, grave diggers are working into the night, as oxygen and vaccines are in short supply. In Europe, countries are slamming their doors shut once again, with quarantines and travel bans. In Bangladesh, urban garment workers fleeing an impending lockdown are almost assuredly seeding another coronavirus surge in their impoverished home villages.
And in countries like South Korea and Israel that seemed to have largely vanquished the virus, new clusters of disease have proliferated. Chinese health officials announced on Monday that they would build a giant quarantine center with up to 5,000 rooms to hold international travelers. Australia has ordered millions to stay at home.
A year and a half since it began racing across the globe with exponential efficiency, the pandemic is on the rise again in vast stretches of the world, driven largely by the new variants, particularly the highly contagious Delta variant first identified in India. From Africa to Asia, countries are suffering from record Covid-19 caseloads and deaths, even as wealthier nations with high vaccination rates have let their guard down, dispensing with mask mandates and reveling in life edging back toward normalcy.
Found this one interesting. I was thinking about the people who have gotten COVID, survived it, and have developed the antibodies naturally. Looks like the Delta variant is so easily spread that many of the un vaccinated with help with getting closer to heard immunity. Me, I would rather be vaccinated, but it looks like herd immunity may happen with or without it:

 www.forbes.com
www.forbes.com

Delta Variant Could Push U.S. Covid Immunity To 85%, Says Former FDA Head
Though it "could be a little worse," the physician predicted Covid will effectively act as a "second circulating flu" this winter.
 www.forbes.com
www.forbes.com
Found this one interesting. I was thinking about the people who have gotten COVID, survived it, and have developed the antibodies naturally. Looks like the Delta variant is so easily spread that many of the un vaccinated with help with getting closer to heard immunity. Me, I would rather be vaccinated, but it looks like herd immunity may happen with or without it:

Delta Variant Could Push U.S. Covid Immunity To 85%, Says Former FDA Head
Though it "could be a little worse," the physician predicted Covid will effectively act as a "second circulating flu" this winter.www.forbes.com
I wonder how this will work.
Something like 58% of Americans are double vaccinated. To get to 85% you need another 27%
If 27% needs to catch it to get to herd immunity, how many people die in the process ?
Currently the 600,000 that died were after 10% of the population caught it. What would 27% of Americans catching it look like ?
I know, I know,... of the 27% some have already caught it. But science tells us the antibodies are there for months, not forever.
They do believe 99% of the people that will die moving forward will be unvaccinated. Too bad something so preventable will happen.
First and foremost, I didn't interview Dr. Gotlieb, I just posted something that I thought was interesting. There are people out there that will not get vaccinated and will get COVID. These are the folks that will as you say "die in the process". that's their choice.I wonder how this will work.
Something like 58% of Americans are double vaccinated. To get to 85% you need another 27%
If 27% needs to catch it to get to herd immunity, how many people die in the process ?
Currently the 600,000 that died were after 10% of the population caught it. What would 27% of Americans catching it look like ?
I know, I know,... of the 27% some have already caught it. But science tells us the antibodies are there for months, not forever.
They do believe 99% of the people that will die moving forward will be unvaccinated. Too bad something so preventable will happen.
"Currently the 600,000 that died were after 10% of the population caught it. What would 27% of Americans catching it look like ?" I don't know, I didn't interview Dr. Gotlieb.
Dr. Gotlieb expressed his opinion and it was uplifting, unlike the crap from the media trying to scare the shit out of you on a daily basis. At least it was some positive news.
Dr. Gotlieb can be reached on The Twitter, maybe you can ask him your questions there:
Yes I put info on vaccine's thread.They do believe 99% of the people that will die moving forward will be unvaccinated. Too bad something so preventable will happen.
Border restrictions, at least for Canadians are starting to ease up a little with more reopening plans in the coming weeks:
 www.usatoday.com
www.usatoday.com
Latest World & National News & Headlines - USATODAY.com
USA TODAY delivers current national and local news, sports, entertainment, finance, technology, and more through award-winning journalism, photos, and videos.
Border restrictions, at least for Canadians are starting to ease up a little with more reopening plans in the coming weeks:
Latest World & National News & Headlines - USATODAY.com
USA TODAY delivers current national and local news, sports, entertainment, finance, technology, and more through award-winning journalism, photos, and videos.www.usatoday.com
He has said several time that the 75% double dose is his metric for the US border.
Yesterday he was talking "weeks"
Article was more about easing the restrictions for Canadian travelers. But I get it, cue up the Debbie Downer music, always negative.He has said several time that the 75% double dose is his metric for the US border.
Yesterday he was talking "weeks"
Article was more about easing the restrictions for Canadian travelers. But I get it, cue up the Debbie Downer music, always negative.
Please explain how saying it's a question of weeks is a downer.

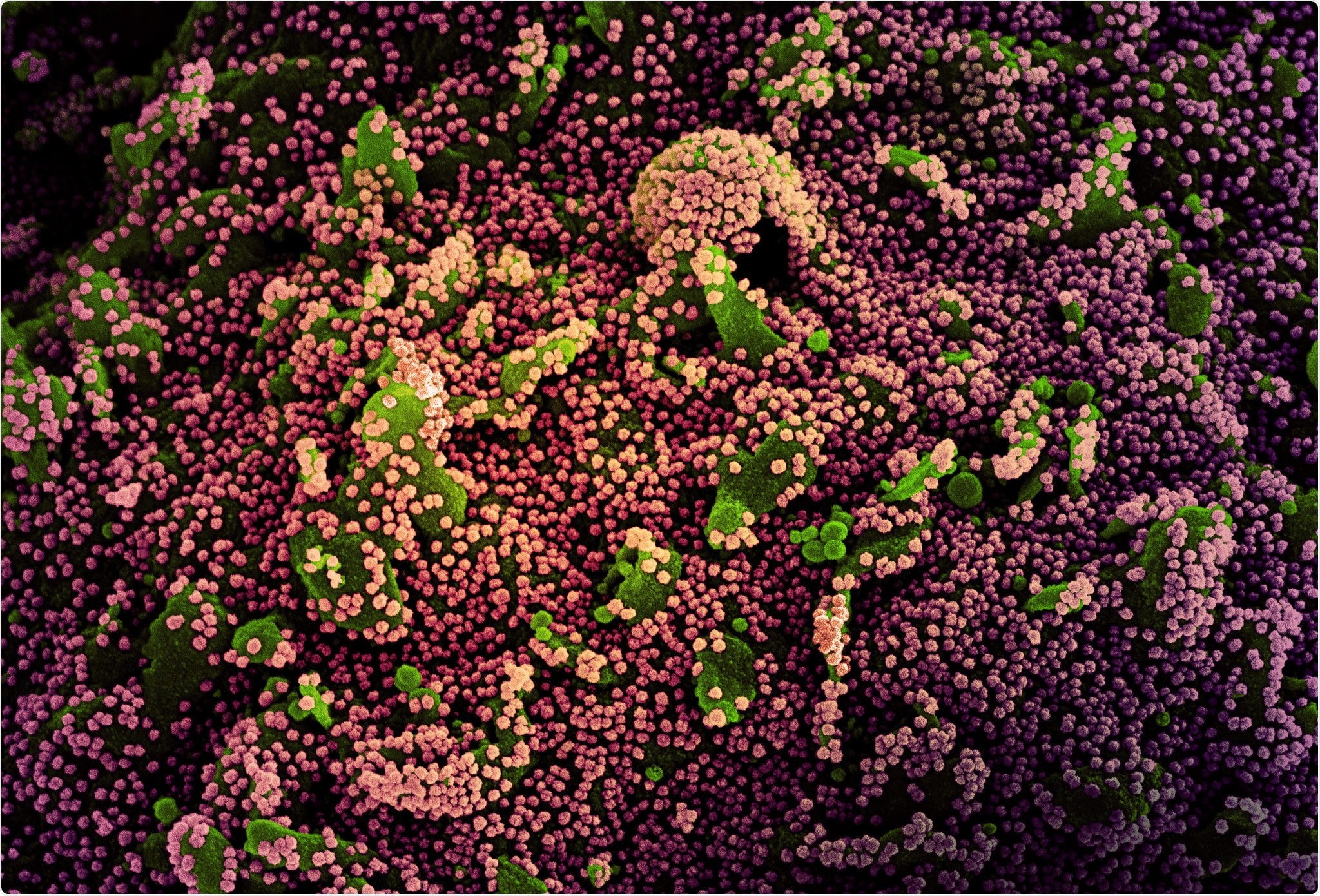
The Lambda COVID-19 variant: What do we know about it?
A recently designated COVID-19 variant of interest by the World Health Organization is coming under scrutiny as more cases are being detected in multiple countries, and amid concerns that it carries mutations that could potentially make it more resistant to antibodies.
A recently designated COVID-19 variant of interest by the World Health Organization is coming under scrutiny as more cases are being detected in multiple countries, and amid concerns that it carries mutations that could potentially make it more resistant to neutralizing antibodies.
The newly labelled Lambda variant, or C.37, was first detected as early as last August 2020 in Peru and was being monitored as an alert for some time prior to its new designation. As of mid-June, the variant had been detected in 29 countries or territories with a particularly high prevalence in South America.
“Lambda has been associated with substantive rates of community transmission in multiple countries, with rising prevalence over time concurrent with increased COVID-19 incidence,” the global health agency wrote in its Weekly Epidemiological Update published on June 15.
“Lambda carries a number of mutations with suspected phenotypic implications, such as a potential increased transmissibility or possible increased resistance to neutralizing antibodies.”
The one and only way to stop these new variants is through vaccination.
Similar threads
- Replies
- 61
- Views
- 11K
- Replies
- 70
- Views
- 39K
- Replies
- 251
- Views
- 46K
- Replies
- 108
- Views
- 22K






